When Was The Cure For Tuberculosis Found? The quest to conquer tuberculosis, a disease that has plagued humanity for millennia, is a complex and ongoing story. This journey, marked by breakthroughs and setbacks, reveals not just the scientific advancements in combating the disease, but also the crucial role of public health initiatives and the persistent challenge of drug resistance.
From ancient remedies to the discovery of streptomycin and beyond, the fight against TB continues to shape medical history and public health strategies worldwide.
This exploration delves into the historical timeline of TB treatment, highlighting key milestones such as the discovery of streptomycin and the subsequent development of other crucial anti-tuberculosis drugs. We will examine the mechanisms of action of these drugs, the challenges of drug resistance, and the significant impact of public health measures, including vaccination programs. Understanding the complexities of TB treatment and the ongoing battle against drug-resistant strains is crucial to effectively addressing this global health crisis.
While there’s no single “cure” for tuberculosis, effective treatments emerged in the mid-20th century with the advent of antibiotics. Ironically, the fresh mountain air once touted as a tuberculosis remedy is now enjoyed by visitors to places like Ruidoso Winter Park , a stark contrast to the sanatoriums of the past. Continued research, however, is crucial in combating drug-resistant strains of this persistent disease.
The History of Tuberculosis Treatment
Tuberculosis (TB), a disease caused by the bacterium Mycobacterium tuberculosis, has plagued humanity for millennia. Its treatment history is a testament to scientific progress, marked by periods of limited understanding and devastating mortality, followed by breakthroughs that dramatically altered the course of the disease. From ancient remedies to modern drug regimens, the journey to combatting TB has been long and complex.
Early Tuberculosis Treatment Methods
Early treatments for tuberculosis were largely ineffective and often based on folk remedies and rudimentary medical practices. Ancient civilizations recognized the contagious nature of the disease, but lacked the understanding of its bacterial cause. Treatments often focused on improving general health and addressing symptoms rather than directly targeting the infection. These methods included herbal remedies, bloodletting, and rest cures, offering little impact on the disease’s progression.
Timeline of Significant Milestones in TB Research and Treatment
| Date | Event | Key Figures | Impact |
|---|---|---|---|
| 1882 | Robert Koch identifies Mycobacterium tuberculosis as the causative agent of TB. | Robert Koch | Revolutionized understanding of TB, paving the way for targeted treatments. |
| 1943 | Streptomycin, the first effective antibiotic against TB, is discovered. | Selman Waksman | Marked a turning point in TB treatment, dramatically reducing mortality rates. |
| 1950s-1960s | Development and introduction of other anti-tuberculosis drugs, including isoniazid, rifampicin, and pyrazinamide. | Various researchers and pharmaceutical companies | Enabled the development of multi-drug regimens, improving treatment effectiveness and reducing drug resistance. |
| 1970s-Present | Continued research on new drugs to combat drug-resistant TB strains. | Numerous researchers and pharmaceutical companies | Ongoing efforts to address the challenge of multi-drug resistant TB and improve treatment outcomes. |
Challenges in Developing Effective Tuberculosis Treatments, When Was The Cure For Tuberculosis Found
Developing effective TB treatments has presented numerous challenges. The unique characteristics of M. tuberculosis, such as its slow growth rate, ability to persist in a dormant state within host cells, and propensity to develop drug resistance, have all hampered treatment development. Furthermore, the global distribution of TB, particularly in resource-limited settings, poses significant logistical and economic hurdles to effective treatment implementation and research.
The Discovery of Streptomycin
The discovery of streptomycin by Selman Waksman and his team at Rutgers University in 1943 marked a pivotal moment in the fight against tuberculosis. Waksman, a microbiologist, systematically screened soil samples for antibiotic-producing microorganisms. This painstaking process led to the isolation of Streptomyces griseus, a bacterium that produced streptomycin, a compound with potent activity against M. tuberculosis.
Impact of Streptomycin on Tuberculosis Mortality and Morbidity
Source: jpabs.org
Before the advent of streptomycin, tuberculosis was a leading cause of death worldwide. The introduction of streptomycin significantly reduced mortality and morbidity rates, offering the first effective treatment option for this devastating disease. While not a complete cure, streptomycin provided a crucial tool for managing the infection and improving patient outcomes. Its impact was particularly profound in reducing the severity and duration of illness.
Comparison of Streptomycin with Other Early Antibiotics
Streptomycin was initially the most effective antibiotic against TB, but it had limitations. Compared to later drugs like isoniazid and rifampicin, streptomycin was less potent and had more significant side effects, including hearing loss and kidney damage. However, its discovery paved the way for the development of more effective and better-tolerated anti-tuberculosis drugs.
Development of Other Anti-Tuberculosis Drugs: When Was The Cure For Tuberculosis Found
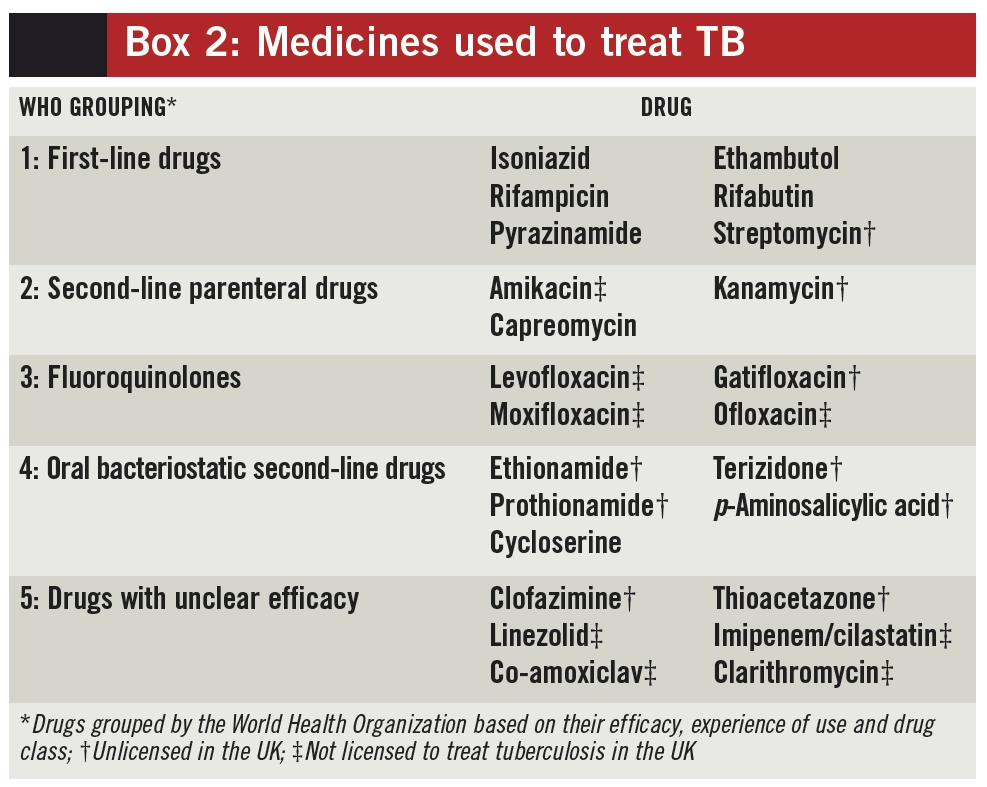
Following the success of streptomycin, a concerted effort led to the development of other anti-tuberculosis drugs. These drugs, when used in combination, significantly improved treatment outcomes and reduced the emergence of drug resistance.
- Isoniazid (INH): A highly effective drug that inhibits mycolic acid synthesis, a crucial component of the M. tuberculosis cell wall.
- Rifampicin (RIF): Inhibits bacterial RNA polymerase, preventing transcription and bacterial growth.
- Pyrazinamide (PZA): Its mechanism of action is not fully understood, but it is particularly effective against actively dividing bacteria.
- Ethambutol (EMB): Inhibits arabinosyl transferase, an enzyme involved in cell wall synthesis.
Mechanisms of Action and Challenges in Drug Development and Resistance
The mechanisms of action of these drugs vary, but they all target essential processes in M. tuberculosis metabolism and growth. However, the development of drug resistance remains a major challenge. The slow growth rate of M. tuberculosis and its ability to persist in a dormant state make it difficult to eradicate the bacteria completely. The emergence of multi-drug resistant (MDR) and extensively drug-resistant (XDR) TB strains necessitates the ongoing development of new drugs and treatment strategies.
The Role of Public Health Measures
Public health initiatives have played a crucial role in controlling the spread of tuberculosis. These initiatives include vaccination programs, screening and case detection, contact tracing, and infection control measures in healthcare settings. A multi-pronged approach is essential for effective TB control.
Impact of Vaccination Programs (BCG)
The Bacille Calmette-Guérin (BCG) vaccine is a widely used vaccine against tuberculosis, primarily in children. While its effectiveness varies depending on factors like the strain of M. tuberculosis and the recipient’s immune status, BCG vaccination has contributed to a reduction in severe forms of TB, particularly in children.
Public Health Campaign to Promote TB Awareness and Prevention
A successful public health campaign would utilize various channels, including public service announcements (PSAs) on television and radio, educational materials distributed in schools and community centers, and social media campaigns to raise awareness. Key messages would include the importance of early diagnosis and treatment, proper hygiene practices, and the benefits of BCG vaccination. The campaign would also address common misconceptions and stigma associated with TB.
The Ongoing Fight Against Tuberculosis
Despite significant advances in treatment, tuberculosis remains a major global health problem. The emergence of drug-resistant strains and the challenges of effective treatment in resource-limited settings continue to hinder eradication efforts. A concerted global effort is crucial to address these challenges.
Multi-Drug Resistant Tuberculosis (MDR-TB)
Multi-drug resistant tuberculosis (MDR-TB) refers to strains of M. tuberculosis that are resistant to at least isoniazid and rifampicin, the two most potent first-line drugs. MDR-TB is significantly more difficult and expensive to treat, requiring longer treatment regimens with less effective drugs. The emergence of extensively drug-resistant (XDR) TB, resistant to even more drugs, further complicates treatment.
Cellular Mechanisms Involved in the Development of Drug Resistance
The development of drug resistance in M. tuberculosis is a complex process involving several mechanisms. Mutations in genes encoding drug targets can reduce the effectiveness of drugs. Efflux pumps can actively expel drugs from the bacterial cell, reducing intracellular drug concentrations. Changes in cell wall permeability can also reduce drug entry into the bacterial cell. These mechanisms can occur independently or in combination, leading to the emergence of drug-resistant strains.
A detailed illustration would show a M. tuberculosis cell with various components labeled, highlighting mutations in drug targets, efflux pumps, and altered cell wall permeability. The caption would explain how these changes contribute to the development of drug resistance, emphasizing the complex interplay of genetic and environmental factors.
Misconceptions about a “Cure” for Tuberculosis

Source: amazonaws.com
A common misconception is that there is a single “cure” for tuberculosis. In reality, TB treatment is a complex process that involves a combination of drugs administered over a prolonged period. The duration and specific drug combination depend on various factors, including the patient’s immune status, the severity of the disease, and the presence of drug resistance.
Complexities of Tuberculosis Treatment Regimens and Adherence
Effective TB treatment requires strict adherence to the prescribed regimen, which typically lasts for several months. Treatment interruptions or incomplete courses can lead to treatment failure and the emergence of drug resistance. The complexities of the treatment regimens, coupled with potential side effects of the drugs, can make adherence challenging for some patients.
Different Stages of Tuberculosis Treatment
TB treatment typically involves an intensive phase, where multiple drugs are administered daily for several months, followed by a continuation phase, where fewer drugs are given for a longer duration. The intensive phase aims to rapidly kill actively dividing bacteria, while the continuation phase targets persistent bacteria and prevents relapse. The specific duration and drug combination for each phase are tailored to the individual patient’s needs.
Final Thoughts
The search for a “cure” for tuberculosis reveals a nuanced reality: there’s no single magic bullet. Instead, success hinges on a multi-pronged approach encompassing effective drug regimens, rigorous adherence to treatment protocols, and robust public health interventions. While significant progress has been made, the emergence of multi-drug resistant TB underscores the need for continued research, innovative treatment strategies, and sustained global commitment to finally eradicate this devastating disease.
The ongoing fight against TB highlights the intricate interplay between scientific advancements, public health initiatives, and the persistent challenge of adapting to evolving strains.
